Welcome to the ACBS Online Peer Supervision Group: Connect online, Support and Learn with your Peers
Submitted By Em Perera, October 27, 2017
Do you want to learn how to become more skilled in using ACT, connect and gain support from other ACBS-members online? Then, please read on!
The ACT Peer Supervision Group is a global forum that aims to provide supervision between colleagues on the experiential practice of ACT in a supported and safe group environment. The groups are hosted and facilitated by Peer Facilitators via Zoom, a video conferencing service. The Peer Facilitators are volunteers within the ACBS community who are committed to providing a forum for collaborative learning to expand their skills and help others as ACT therapists. These meetings are free to all ACBS members. They provide an opportunity to meet other ACT practitioners from around the world to share our knowledge and our struggles in practicing within the ACT model.
Since it’s inception in 2015, there have been two formats for online peer supervision at ACBS. First, is a drop-in format where anyone who has completed the free online registration can come along to the fortnightly meetings. At the moment these run only on Fridays but could be extended if there is interest for different days and times (see below for upcoming meeting dates in 2017). At the drop-in group you will usually see familiar faces, but you may also meet some new people who have come along. The second is a closed group (the same group members meet each week) for a set number of weeks. Both formats are inspired by the Portland Model of Peer Consultation (see below), but with a few adaptations to make it easier to run the groups on-line (as opposed to in the same physical space).
Peer-Supervision Drop-in Groups in 2017, Meetings on Fridays at 7am and 10am Eastern Standard Time
Nov 10, 2017
Nov 24, 2017
Dec 8, 2017
Dec 22, 2017
Benefits of our online peer supervision
Opportunity to learn from ACT practitioners from around the world: ACT is a relatively new approach, so it can feel isolating using this approach without the support of colleagues nearby to discuss cases and check out your therapeutic decisions. There are however, people practicing ACT in different parts of the world. This ACT peer supervision group allows us to pool this community, so that we can learn from one another. Thus creating a community network of people collaboratively learning, supporting and sharing knowledge.
Low-Cost: The peer supervision groups are free for ACBS members. Attending ACT workshops are extremely useful, especially early on to learn about the model and meeting other people who use it with similar clients to you. Regular supervision and skills practice is essential for continued professional development, but the financial cost of weekly and fortnightly supervision, can be a real barrier to practitioner development. This is particularly true for those in private practice. These peer supervision groups provide a forum for practitioners, at all skill levels, to practice their knowledge and hone their ACT skills without the financial burden.
Transparent and shared roles: Finding an individual supervisor, who is able to adequately support your skills development and growth requires research, trial and error, and luck. Peer supervision allows people at all levels (from ACT trainers to people curious about how ACT works in practice) to meet and share their experiences and participate in safety in order to grow personally and professionally. As peers everyone in the group (including facilitators) take turns in the different learning roles: to give and receive feedback and grow.
Convenient: We cater to different needs that ACBS-members have. While sharing the wish to learn from and with peers, we all differ in terms of agenda’s, duties, mobility, time availability and geographical areas are just a few things that can be a real hurdle to participate in face-to-face peer meetings. Online peer meetings can take away some of these barriers. Moreover, since we offer two different formats, we cater to different learning needs and availability of members. For example: Our drop-in peer supervision meetings are held every two weeks and you are free to attend any or all of the meetings with changing participants. Our closed group peer supervision meetings, on the other hand, offer participants a way to work for several consecutive weeks with the same participants. Depending on your personal situation, one might be a better fit than the other.
Friendly, caring and supportive environment: Growing personally and professionally requires revealing to others our gaps in knowledge or experience, which can feel difficult and can make us feel vulnerable. The facilitators of the peer supervision groups are aware of this and work to create a warm, welcoming and supportive environment that allows everyone to give and receive guidance and feedback in a positive and respectful way.
Experiential learning: Reading, hearing or watching someone doing ACT gives us some idea about this approach, but it is through the actual practice of using the different elements within the ACT Hexaflex that deeper understanding, learning and growth takes place. These groups provide an opportunity to learn through experiential practice that is not readily available through books and workshops. All of our facilitators are trained and aware of the goal to keep the meetings as “experiential” as possible and will help the group to stay on track.
Facilitator’s role in the drop-in meetings
Maintain the structure for the meeting and ensure the group moves smoothly along throughout the 90 minutes.
Invite and encourage participants to take part in exercises and facilitate the discussion afterwards to draw out learning from the experience.
Be willing to take compassionate risks for the group and their own development.
Be aware that they do not need to be experts in ACT but will knowledgeable and dedicated to ACT processes and make an effort to maintain the ACT therapeutic stance.
Format of the Drop-In meetings
We are aiming to create a radically experiential supportive learning environment for all participants. Meetings are structured into four main parts to help maintain the purpose and focus for the group to learn ACT:
1. Mindful Connection The facilitators ask for a volunteer to lead a brief mindfulness exercise, which would include some or all of the Hexaflex* processes, followed by brief feedback if desired.
2. Fish Bowl Real Play This is the main part of the meeting. This is an opportunity for group members to practice their ACT skills by stepping into the ‘therapist/Skill Builder’ role and help another group member with a supervision issue, either concerning a particular client or a personal growth issue. Other group members can volunteer to provide advice/support to the Skill Builder or be Hexaflex Monitors, who observe the processes and offer feedback at the end of the ‘Real Play’.
3. Feedback At the end of the ‘real play’ session Initially the Skill Builder & Supervisee pair are invited to share how they experienced the Real Play. Then other peers are invited to say how they experienced it and provide ‘supportive feedback’. This consists of 3 components: 1. Personal appreciation (what you admired) 2. Your emotional reaction to what you heard. 3. Curiosity about the direction the ‘therapist’ took within the ACT Hexaflex model.
4. Wrap-up The meeting closes with members sharing one word to describe their experience of the meeting, and/or the committed action to practice before the next meeting?
Even though each group is unique due to its drop-in nature, this structure helps to guide the meetings. We find it is helpful in promoting learning and provides safety for participants to know it’s structure to join in as and when they are able.
How can you join these meetings?
STEP 1: Register. This is a one-time registration allowing you to drop-in on days and times that work for you. Following registration you will receive a welcome email that has the Zoom number for you to enter the meeting. https://www.surveymonkey.com/r/ZCCM25R
STEP 2: Check your time zone As the meeting times are in different time zones, we ask that you check what time the meetings take place in your time zone. Please note that the dates for summer and wintertime changes vary from country to country, do check when your time changes.
Additional guidance
Commit to the entire 90 minutes. As a courtesy to others and minimize disruption during the meeting we ask members to commit to the entire 90mins. We suggest that you arrive 5mins before the start time to log on. Access to the meeting is locked 5mins after the start time but you can always try again at the next meeting in two weeks. If you have trouble logging in or other questions please email us at [email protected].
Respect Confidentiality in the group. You will appreciate that a safe environment is essential for participants to use the supervision effectively and enable professional growth. So we ask that you don’ share the content of these groups outside the group.
Closed 6-Week Group
The advantage of the closed group is that there is an exact start and end date and consists of 6 consecutive weekly meetings. In contrast to the Drop-In Peer supervision meetings, the meetings are lead by two permanent facilitators and participants commit to attend all six meetings. As with the drop-in group there is in-depth, experiential practice of ACT skills based on the Portland model but with a stable group of co-participants. We do not have dates for a closed group at present but keep an eye out on the Online ACT Peer Supervision Group page within the ACBS website.
Appendix: Useful documents
ACT therapeutic stance
Portland Model of Peer Consultation, https://portlandpsychotherapytraining.com/acceptance-and-commitment-therapy-peer-clinical-consultation-group
1. ACT Therapeutic Stance
1) Take an Equal, Vulnerable, Genuine, and Sharing Point of View
2) Model Acceptance of contradictory thoughts and feelings
3) Be Compassionate and Human, Avoiding Criticism and Judgment
4) Bring the issue back to what the self-presenters Experience is showing up
5) Not Arguing Lecturing, Convincing or Coercing
6) Not Explaining the ‘meaning’ of paradoxes or metaphors to develop ‘insight’
7) Willing to Functionally Self-Disclose
8) Avoid canned ACT interventions but tailor interventions to suit the individual needs
9) Demonstrate flexibility to change course to fit those needs in the moment. Allowing new metaphors, exercises, and behavioral tasks to emerge from the presenters own experience and context
These 9 factors can be loosely divided into three overarching functions:
Receiving – Equal, vulnerable, genuine, accepting and defused, compassionate, humanizing and sharing, functional self-disclosure
Workability – Experience as the Guide, not convincing, not coercing, not arguing, not lecturing, not explaining the ‘meaning’
Contextualizing – Avoiding Canned ACT, Changing and Customizing for ‘In The Moment’ Needs.
Acceptance and Commitment Therapy Core Competency Self-Rating Form
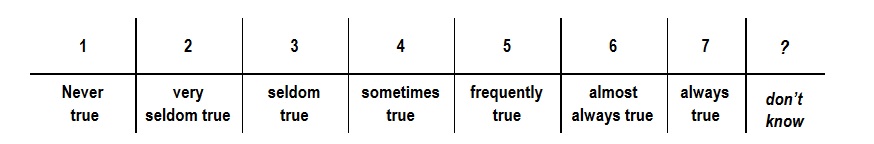
Below are listed a number of statements. Please rate how true each statement is for you when you use ACT, by writing a number next to it. Use the scale below to make your choice.
Core Competencies Involved in the Basic ACT Therapeutic Stance
The basic psychological stance of the ACT therapist is an especially important factor in providing good treatment. This involves being able to make contact with the “space” from which ACT naturally flows, as well as modeling certain facets of psychological flexibility that we seek to impart to the client. Like many treatment traditions, ACT emphasizes the importance of therapist warmth and genuineness. This stance emerges quite naturally from the core understanding of human suffering from an ACT perspective. When we see our clients trapped by language, we see ourselves and the traps which generate our own pain. An “I and thou” perspective is the natural precipitant of this recognition.
Collectively, the following attributes define the basic therapeutic stance of ACT.
1. The therapist realizes that he or she is in the same soup as the client and speaks to the client from an equal, vulnerable, genuine, and sharing point of view ___
2. The therapist models willingness to hold contradictory or difficult ideas, feelings, memories, and the like without needing to “resolve” them. ___
3. The therapist takes a compassionate and humanizing stance toward the client’s suffering and avoids criticism, judgment or taking a “one up” position. ___
4. The therapist always brings the issue back to what the client’s experience is showing, and does not substitute his or her opinions for that genuine experience. ___
5. The therapist does not argue with, lecture, coerce or even attempt to convince the client of anything. If you find yourself attempting to change a client’s mind, stop. You are not doing ACT. ___
6. The therapist does not explain the “meaning” of paradoxes or metaphors to develop “insight.” ___
7. The therapist is willing to self disclose about personal issues when it makes a therapeutic point. ___
8. The therapist avoids the use of “canned” ACT interventions. Interventions are responses to the particular client we are treating. ___
9. The therapist tailors interventions to fit the client’s language and immediate life experience. ___
10. The therapist sequences and applies specific ACT interventions in response to client needs, and is ready to change course to fit those needs at any moment. ___
11. New metaphors, experiential exercises and behavioral tasks are allowed to emerge from the client’s own experience and context. ___
12. ACT relevant processes are recognized in the moment and where appropriate are directly supported in the context of the therapeutic relationship___
Developing Acceptance and Willingness/Undermining Experiential Control
13. Therapist communicates that client is not broken, but is using unworkable strategies. ___
14. Therapist helps client examine direct experience and detect emotional control strategies. ___
15. Therapist helps client make direct contact with the paradoxical effect of emotional control strategies. ___
16. Therapist actively uses concept of “workability” in clinical interactions. ___
17. Therapist actively encourages client to experiment with stopping the struggle for emotional control and suggests willingness as an alternative. ___
18. Therapist uses shifts between control and willingness as an opportunity for the client to directly experience the contrast in vitality between the two strategies. ___
19. Therapist helps client investigate relationship between levels of willingness and sense of suffering willingness suffering diary; clean and dirty suffering) ___
20. Therapist helps client make experiential contact with the cost of being unwilling relative to valued life ends (Are you doing your values; listing out value, emotional control demand, cost, short term/long term costs and benefits) ___
21. Therapist helps client experience the qualities of willingness (a choice, a behavior, not wanting, same act regardless of how big the stakes) ___
22. Therapist uses exercises (jumping; cards in lap, eye contact) and metaphors (box full of stuff, Joe the bum) to help client contact willingness the action in the presence of difficult material. ___
23. Therapists structures graded steps or exercises to practice willingness. ___
24. Therapist models willingness in the therapeutic relationship. ___
25. Therapist detects struggle in session and teaches the clients to do so. ___
Undermining Cognitive Fusion
26. Therapist identifies client’s emotional, cognitive, behavioral or physical barriers to willingness ___
27. Therapist suggests that “attachment” to the literal meaning of these experiences makes willingness difficult to sustain ___
28. Therapist actively contrasts what the client’s “mind” says will work versus what the client’s experience says is working ___
29. Therapist uses language tools (get off our buts, both/and), metaphors (bubble on the head, two computers, monsters on the bus) and experiential exercises (tin can monster) to create a separation between the client and client’s conceptualized experience ___
30. Therapist uses various interventions to both reveal the flow of private experience and such experience is not “toxic” ___
31. Therapist works to get client to experiment with “having” these experiences, using willingness as a stance ___
32. Therapist uses various exercises, metaphors and behavioral tasks to reveal the “hidden” properties of language (milk, milk, milk; what are the numbers?) ___
33. Therapist helps client elucidate the client’s “story” and helps client make contact with the arbitrary nature of causal relationships within the story ___
34. Therapist helps client make contact with the evaluative and reason giving properties of the client’s story (no thing matters, good cup/bad cup) ___
35. Therapist detects “mindiness” (fusion) in session and teaches the client to detect it as well ___
Getting in Contact with the Present Moment
36. Therapist can defuse from client content and direct attention to the moment ___
37. Therapist can bring his or her own feelings or thoughts in the moment into the therapeutic relationship ___
38. Therapist uses exercises to expand the clients sense of experience as an ongoing process ___
39. Therapists tracks content at multiple levels and emphasizes the present when it is useful ___
40. Therapist models coming back to the present moment ___
41. Therapist detects client drifting into past and future orientation and comes back to now ___
42. Therapists teaches the client to do likewise ___
Distinguishing the Conceptualized Self from Self-as-context
43. Therapist helps the client differentiate self-evaluations from the self that evaluates (thank your mind for that thought, calling a thought a thought, naming the event, pick an identity) ___
44. Therapist employs mindfulness exercises (the you the you call you; chessboard, soldiers in parade/leaves on the stream) to help client make contact with self-as-context ___
45. Therapist uses metaphors to highlight distinction between products and contents of consciousness versus consciousness (furniture in house, are you big enough to have you) ___
46. The therapist employs behavioral tasks (take your mind for a walk) to help client practice distinguishing private events from self ___
47. Therapist helps client understand the different qualities of self conceptualization, just noticing events and simple awareness ___
Defining Valued Directions
49. Therapist helps client clarify valued life directions (values questionnaire, value clarification exercise, what do you want your life to stand for, funeral exercise) ___
50. Therapist helps client “go on record” as wanting to stand for valued life ends ___
51. Therapist puts his or her own therapy relevant values in the room and models their importance ___
52. Therapist teaches clients to distinguish between values and goals ___
53. Therapist distinguishes between outcomes and processes ___
54. Therapist respects client values and if unable to support them, finds referral or other alternatives ___
Building Patterns of Committed Action
55. Therapist helps client identify valued life goals and build an action plan ___
56. Therapist encourages client to “have” barriers and make and keep commitments ___
57. Therapist uses exercise and non traditional uses of language to reveal hidden sources of interference to committed actions (fish hook metaphor, forgiveness, who would be made right, how is your story every going to handle you being healthy) ___
58. Therapist encourages client to take small steps and to look at the quality of committed action ___
59. Therapist keep clients focused on larger and larger patterns of action ___
60. Therapist integrates slips or relapses into the experiential base for future effective action ___
